Disclaimer: Any views expressed by individuals and organisations are their own and do not in any way represent the views of The Heritage Portal. If you find any mistakes or historical inaccuracies, please contact the editor.
In 1994, the article below appeared in the Sandton Historical Association Annual Magazine. It provides a glimpse of primary health care in Witkoppen, now an outlying area of Johannesburg but previously part of Sandton. The author, Dr Margaret Fouche, one of the doctors who worked at the clinic, allowed the Association to use the material for the article from her longer and more detailed history of the clinic.
Together with the article by Agnes Kulenkampff on Witkoppen School, published in the Association’s Magazine of 1978, and reproduced on the Heritage Portal (click here to read), readers will gain a sense of the deleterious conditions of life for Africans in our region in past decades, but also of the strength of volunteer assistance and contributions.
The early years
The Witkoppen Clinic has been in operation for nearly fifty years, and it seems appropriate to write an account of it while some of the original workers can help with their recollections. Since the Witkoppen School and the Clinic have always been connected, and since the School preceded the founding of the Clinic a brief account of the school's beginning is given here.
Sketch of the Witkoppen School buildings (via the Annual Magazine of the Sandton Historical Association)
The Witkoppen School began in 1942 when Mr. H.K. Mapoeloa began teaching in a room in an old farmhouse. The land belonged to Mr George Mason who later sold his farm but reserved two acres for the “local native people so they might keep their school and build a community centre”. Because Africans at that time couldn't own land in “white” areas, ownership was vested in the Anglican Board of Trustees. The church built a new school and in April 1943, Bishop Geoffrey Clayton dedicated it “to the glory of God and in honour of St Justin”. The name thus became St Justin’s and the school was formally constituted as a mission school. This circumstance was to lead to a grave crisis ten years later.
When the Bantu Education Act was passed in 1953, Bishop Ambrose Reeves refused to accept the syllabus which the Department of the Interior decreed was mandatory for all schools teaching African pupils and he decided to close all mission schools in his diocese. The parents of St Justin’s, however, opposed this decision and sent a deputation to the then Minister of Native Affairs. Representatives of the Department visited the school and on 28 March 1955 declared that the school could continue under lay management. In this way, St Justin’s became the Witkoppen Farm School, and it has remained so.
It was in a classroom of this school that a number of public-spirited nurses began the Witkoppen clinic in 1946. They included Catherine Payne, Kathleen Breeze, Beth Withinshaw and Cynthia Howard. Mrs. Payne had before then been helping the poor people of the neighbourhood by seeing them and treating them in her own house. In 1946 she and her two colleagues, together with Mrs. Alexander, a physiotherapist, took over a classroom at Witkoppen School on Friday afternoons. Their husbands helped by raising money for medicines and dressings. Later they were joined by the Witkoppen Clinic’s first three doctors: Dr Sue Hulme, Dr Marioth Coster and Dr Louis Smuts.
The clinic numbers grew rapidly, and the classroom was clearly quite inadequate. There was no examination couch, and everything had to be packed away after each session. In 1950 Dr Schneider, a neighbouring landowner, allowed the clinic to use a small farmhouse on his property, between the Fourways crossroads and the school. The building was old and dilapidated, without light, water or lavatory. The Bryanston road was said to be perilous after clinic sessions, with all the workers speeding home to the loo! The sitting room of the house became the adult consulting room – it had French windows (not much glass in them) opening onto an uncut lawn. In fact, the grass was high enough to hide the skokiaan factory run by some of the workers! The dressing room was in the middle of the house and was very dark. Paraffin lamps were sometimes needed, and sterilizing was done on Primus stoves. There was a great deal of sterilizing required in those days because syringes were made of glass with metal plungers and even the hypodermic needles were boiled and had to be used over and over again.
The dispensary was in the old kitchen of the house. Children were seen in what was probably the pantry – just large enough for a chair for the doctor, a table for a scale, and a backless stool for the mother – it had to be backless so that a large portion of her body could protrude into the passage! Later this department moved on to the stoep where there was a table, an examination couch, chairs, a screen, and benches for waiting mothers – a much more pleasant working place but sometimes patients were seen outside.
The staff made themselves as comfortable as possible in these difficult circumstances. Walls were whitewashed, shelves were erected, tables, chairs, benches, curtains, tiles, and clothes, were found and added to the furnishings. Water had to be brought in and everyone had a bowl of water/Dettol mixture handy for dipping their fingers into between patients. Whether this made the fingers cleaner or dirtier towards the end of a morning is anyone's guess!
Two new doctors soon joined the original three: they were Dr Nina Abelheim in 1956 and Dr Margaret Fouche in 1957. Drs Hulme and Fouche saw children and the others saw adults. Dr Coster and Hulme also ran a branch of the Family Planning Association which had official approval, but which was run on private donations. There were no contraceptive pills in those days and caps had to be fitted and jelly supplied. Dr Coster did the administrative work until she joined the Johannesburg City Council in 1961 when Dr Smuts took over.
At that time the clinic was open on Tuesday and Friday mornings and each doctor came once a week. The card office was most efficiently trained by Mrs Nora Trew whose husband, Anthony, was the first treasurer. The chief interpreter for the offer was Violet. It was not certain what her nationality was, but she had an extensive and colourful vocabulary in English and Afrikaans and was equally fluent in several Black languages. She kept the patient strictly in order and knew exactly who deserved free treatment and who did not. Violet was one of the chief brewers and made frequent sorties into the long grass to taste her product, so towards the end of the morning she was not as sober as when she started.
The first pharmacist at the Clinic was Mrs. Edna Gordon-Grant. She and her sister. Mrs Doreen McKie, used to go out at weekends and bottle medicines helped by Dr Coster whose small daughter was allowed to put the corks in the bottles.
There were many nursing sisters on the clinic roster, some semi-trained Red Cross and St John Ambulance, and some quite untrained. The doctors and nurses had seen it all before, but tribute should be paid to the semi- and untrained women who worked in the dressing room.
Funds were raised by many friends of the Clinic by jumble sales, sales of books, Christmas cards, and cakes. Some drugs and supplies were donated, but most had to be bought. The Johannesburg municipality provided vaccines for immunising the children, and the Family Planning Association gave birth control necessities. There was some income from the patients too.
The patients came in ever increasing numbers, rising to 5039 in 1958. They came on foot, by bicycle, by donkey cart, or in their employer’s cars and some traveled great distances. If they could not pay, the charge was one shilling for adults and sixpence for children; if not they were seen without fee. Food for the underfed and clothes for the needy were provided when available, and there was milk for malnourished children.
For 14 years Witkoppen Clinic operated under these primitive conditions. They were very busy but happy years for the staff, who did not seem worried about the anomaly of practising “bush” medicine within a short distance of the great city of Johannesburg. Witkoppen Clinic was providing primary healthcare before the term was invented.
1963: A new clinic
In November 1963 President John F. Kennedy of the United States was assassinated and his death affected so distant and so insignificant organisation as the Witkoppen Clinic. Charles W. Engelhard Jr, the chairman of Rand Mines, on one of his periodic visits to South Africa, decided he would like to build a memorial to his friend the President. The Blakeways, a family who lived nearby, had interested him in the Witkoppen School and he agreed to finance a hall and Chapel for the school. After a little further persuasion, the building was enlarged to include space for the Clinic, with a waiting room which could form an extension to the school hall. So the west end of the school came to comprise an interdenominational chapel and the east end the clinic, thus providing spiritual and physical healing under one roof. In the Chapel is a tablet commemorating President Kennedy believed to be his only memorial in Africa.
There was a grand opening ceremony for the new J.F. Kennedy memorial building in 1964. The Bishop of Johannesburg consecrated the chapel and there were speeches by the school principal Mr. Samson Matlou, and a member of the Department of Education and Training.
The Chapel (The Heritage Portal)
Compared with the old cottage, the new clinic building was luxurious. There was running water, which meant that there were wash basins and a flush toilet. There was electricity, providing power for lights and the sterilizer for instruments, a kettle for tea, and heaters in winter. To begin with there was an office, a large washing room and dispensary, three consulting rooms, and a dressing room. The building was extended twice, each time with the help of a generous donation from the Engelhard Trust.
Four of the doctors from the cottage came over to the new clinic: Drs Smuts, Abelheim, Hulme, and Fouche. Dr Jill Home was enlisted next—she began the ante-natal section and also treated adults medically. At this time, adults paid 20c and children 10c, when an employer brought a patient the charge was 50c. This covered consultation, injections and medicine. Those who could not pay were still treated free and were given the bus fare to return if further treatment was required.
The clinic is threatened
A few years later, in 1967, a letter from the Transvaal Board for the Development of Peri-Urban Areas advised that the clinic could not continue to see “Bantu” patients without the approval of the Minister of Bantu Affairs, and that written application for this approval and full details of the clinic must be submitted forthwith. The application was duly made, and a couple of weeks later followed the most nerve-wracking inspection. On each clinic day there would be one or two grim-looking officials from the State Health Department, sometimes one would be a woman, but she looked pretty grim too. They watched, they poked around, they criticised the nursing staff for not wearing epaulettes, they had to be satisfied about the poison register and the locking up of habit-forming drugs. Nothing pleased or amused them. They would not even have a cup of tea. The only aspect that seemed to strike a chord was the Family Planning Association, so that was mentioned several times a day, although in fact it only used the premises once a week.
After a long wait of six months a verdict was given. Ministerial approval was granted “to conduct the above-mentioned clinic, subject to the condition that this approval may at any time be withdrawn by the Minister at his discretion”. Not a word of thanks for the good work of the clinic and certainly no offer of help! However, Witkoppen Clinic fared better than the Margaret Ballinger Home for mentally handicapped Black children – the only one in the Transvaal at the time. After 27 years it was told by the Department of Bantu Administration and Development that it must close down “because it was in a white the area.”
A new crisis
For nearly ten more years the work of the Witkoppen Clinic continued and by 1979 the number of patients at each session had increased to about 200. However, it was becoming more and more difficult to find doctors who were prepared to work voluntarily at the clinic. The Sandton Town Council was approached, but it felt that it could not support the clinic because most patients came from outside Sandton. The next move was to ask the Surgeon-General of the South African Defence Force whether any of his medical officers could help out once or twice a week, but this was not possible. Edenvale Provincial Hospital was also approached but it, too, could not assist.
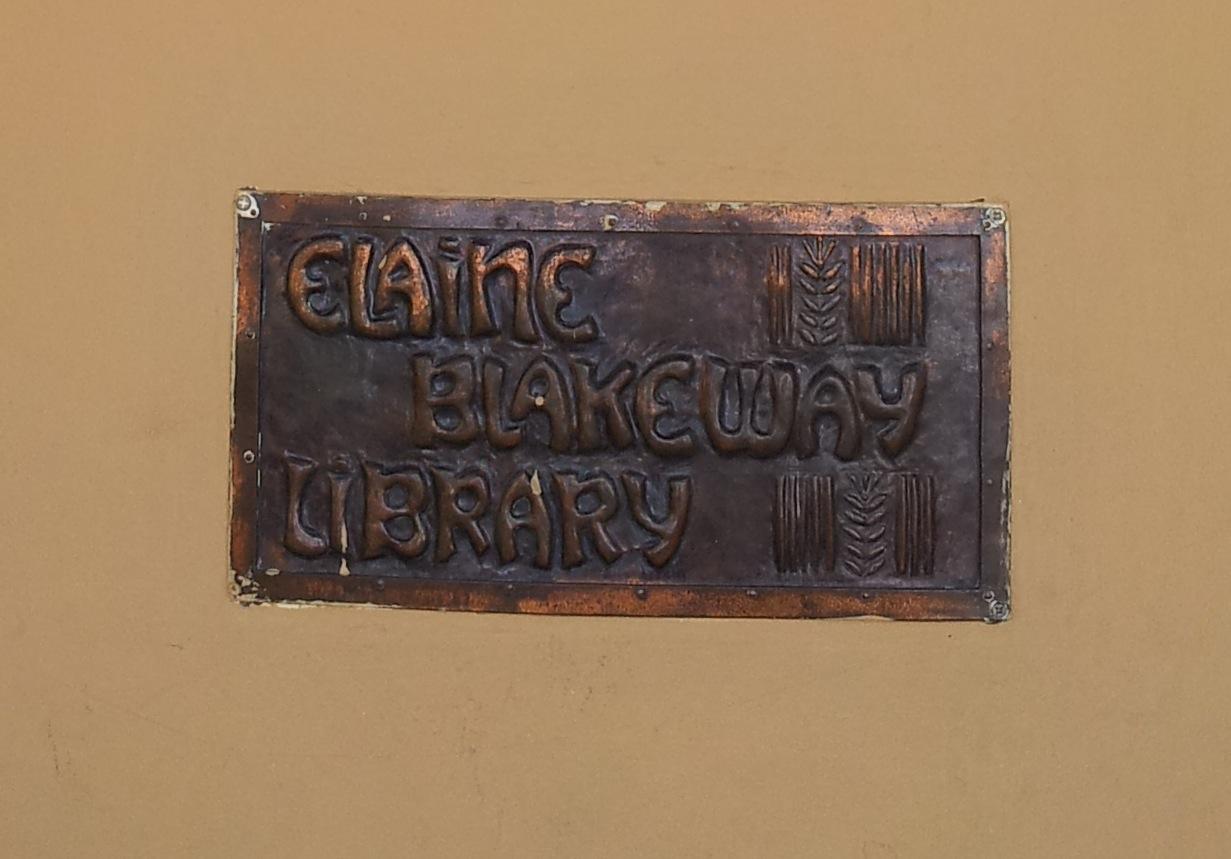
Thus on 3 July 1979 a notice of closure was put up on the clinic door, and the patients were told that the clinic would cease. it was at this stage that Mrs. Elaine Blakeway stepped in. She and her husband lived near the clinic and had always played an active part in its affairs and those of the school. Mrs. Blakeway was determined that the clinic would continue and she called a meeting of all the workers to discuss the matter. She enlisted the help of Mr Hank Slack who also lived nearby, held meetings in his house and, helped by his wife Mary (née Oppenheimer), he became an energetic fundraiser. The clinic owes him a deep debt of gratitude for coming to the rescue and for making it possible to pay some of the workers so that the operation became viable again.
Commemorating Elaine Blakeway (The Heritage Portal)
A full-time administrative sister and a full-time resident sister were appointed, and a house was built for the latter on Mr Slack's property opposite the clinic. Money was provided for doctors from Soweto to come once a week. Two pharmaceutical companies paid the salaries of one doctor and a nursing sister to work at one session a week.
The work goes on
The work of the Witkoppen Clinic has continued with support from various sources. A group of nurses at the Johannesburg hospital collected R800; a bakery denotes bread for the patients twice a week; money, drugs, and food parcels come from others; a man who imports second hand clothes from Europe sends the clinic a bundle each winter. The Witkoppen School, next door, has also helped in many ways, at one time allowing the clinic to use their telephone and the manual labour of pupils.
There have been many changes over the years. and in particular the state of the patients. Today there is far less malnutrition, and whereas in the early days there were sometimes children with fully developed kwashiorkor, more recently the cases have diminished. Diphtheria was once extremely frequent, and today measles, although sometimes seen, is not as severe as it was in the past. Tuberculosis still occurs but the state health caravan for X-rays and treatment calls regularly. Leprosy is on the decrease. AIDS is, of course, the spectre of the future, but everything possible is being done in the field of education and the free supply of condoms. Gastro-enteritis is common, especially in summer, but fewer children now need to be hospitalized. All children are checked as soon as possible after birth for congenital defects and immunization programs are routine.
Running the clinic is hard work for the staff, with around 250 patients each clinic day, but Witkoppen Clinic has always been a happy, friendly place. Recently, more buildings have been added with more modern facilities. In these changing times it is hoped while there are people who need help the Witkoppen Clinic will always be there with people to help them.
Thank you to Jane Carruthers for finding, transcribing and editing this article.
Main image: Witkoppen Clinic and School from above via Google Maps
Comments will load below. If for any reason none appear click here for some troubleshooting tips. If you would like to post a comment and need instructions click here.